Lumbar Disc Herniation
Lumbar Disc Herniation
Lumbar Disc Herniation
Although disc herniation is a feared condition, most people can return to their daily lives within one or two weeks or months without the need for surgery. Although some of the symptoms persist, most people become functional.
You should receive medical support as early as possible so that your doctor can give you the appropriate medical treatment, exercises, physical therapy, correct body movements, and physical activities. An accurate diagnosis and early treatment will enable a more rapid recovery. Use all medicine as described by your doctor. Report changes in your symptoms so that your doctor can adjust them accordingly. If you begin to lose control of your bladder and bowel in addition to pain, or if you have numbness around your anus or genital area, inform your doctor immediately.
What Is a Disc Herniation?
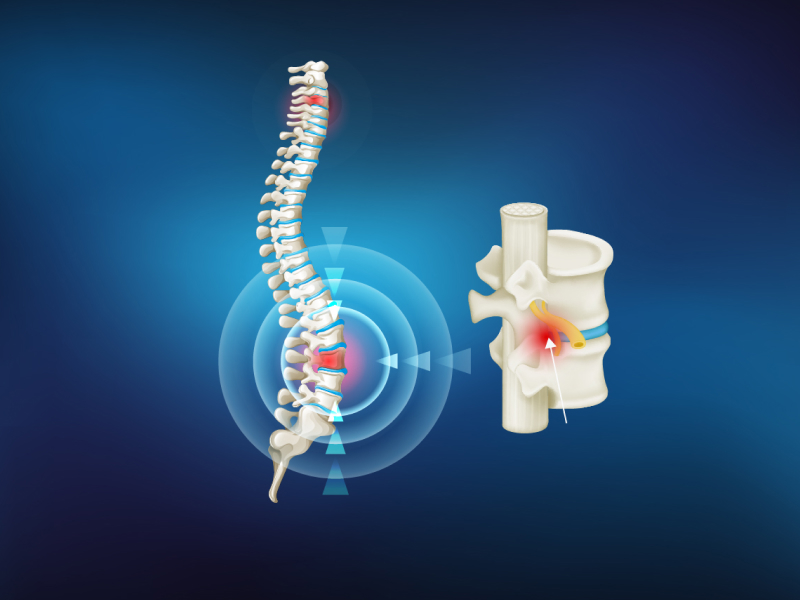
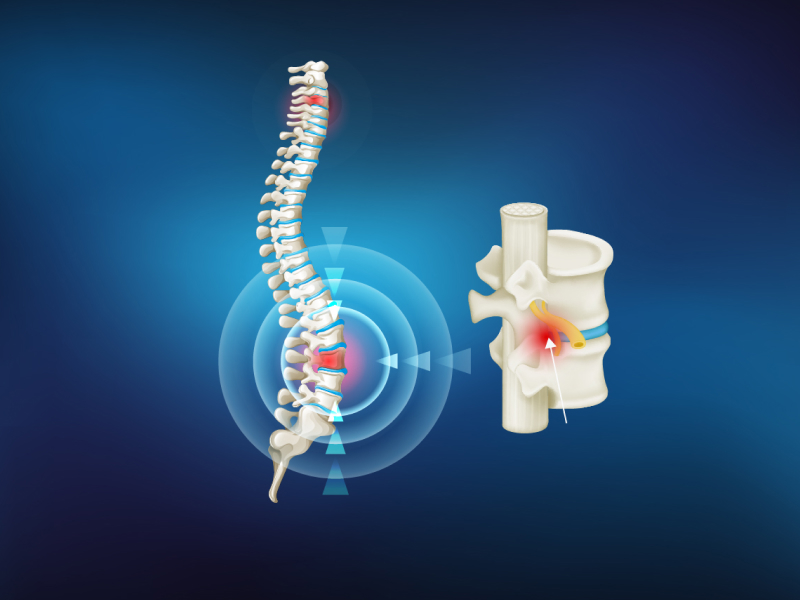
The spine is composed of a chain of bones, called vertebra, connected to each other. The vertebras surround the spinal cord and protect it from injury. The nerves exit the spinal cord and travel to other areas of the body to provide the connection between the brain and the rest of the body. The brain moves the muscles via conduction of the messages sent down through the nerves. The nerves also carry sensation, such as pain and heat, to the brain.
The vertebrae are connected to each other with discs and two small joints, named facet joints. The disc that attaches one vertebra to the other is composed of strong connective tissue, and acts like a cushion—a shock absorber like a suspension in cars—between the vertebras.
The discs are composed of a strong outer layer named "annulus fibrosus", and a gelly-like substance in the core, named "nucleus pulposus".
With increasing age, the center of the disc begins to lose water content, and the disc cannot perform its shock-absorbing function as it used to. The outer layer may rupture with further degeneration of the disc. This condition may result in the overflowing (disc herniation or rupture) of the disc core through a tear in the outer layer and into the space that carries the nerves and spinal cord.
The herniated lumbar disc may result in pain, numbness, tingling or weakness due to compression on the nerves in the spinal cord. This condition is called "sciatica" and affects 1-2 percent of people, often between ages 30 and 50. Disc herniation may result in upper back pain as well, however back pain by itself without leg pain may have many causes apart from disc hernia.
What Are Treatment Options?
Most of patients—80 to 90 percent—who experience recent and first-time disc herniation may improve without any treatment. Your doctor will prefer to try nonsurgical treatments in the first few weeks. Despite the completion of treatment, if you continue to have pain that refrains you from your normal activities, then your doctor may suggest surgery. Although surgery may fail to give your leg its former power, it will prevent further loss and stop leg pain. Surgery is often recommended to cure leg pain (successful in more than 90 percent of patients), and is less effective in eliminating back pain.
Non-surgical Treatment in Lumbar Disc Herniation
Your doctor may offer you treatments such as:
If rest is recommended, ask your doctor how long you need bed rest. Bed rest longer than necessary will cause joint stiffness and muscle weakness, making it difficult for you to perform activities that may decrease your pain. Therefore bed rest often does not exceed two days for lumbar pain, and one week for lumbar disc hernia. Besides, lying on a hard surface has no proven efficacy in the management of hernia and pain. Ask your doctor if you can continue to work during the treatment.
In addition, patient education with the help of a nurse or physiotherapist on how you can perform your daily activities without overloading your back may be helpful.
The aim of nonsurgical treatment is to decrease irritation caused by the herniated disc, protect the spine by correcting the general status of the patient, and to increase overall functionality. These goals can be successfully accomplished in most patients with disc hernia, using an organized treatment program that combines numerous treatment methods.
Ultrasonic heat, electric impulses, heat application, cold application, and manual (massage) therapy are among the initial treatments that your doctor may recommend. These treatments may decrease pain, inflammation, and muscle spasm. They will also facilitate an exercise program. Traction (pulling, stretching) may provide slight pain relief in some patients. However, this treatment must be performed only by a physical therapy specialist or a physiotherapist. People who are not licensed to do this may cause irreversible harm. In some cases, your doctor may recommend you to use a lumbar brace (a soft and flexible back support) at the beginning of your treatment. However, these braces do not heal the herniated disc. Treatment applied with the hands (manipulation) may provide short-term relief in vague lower back pain.
A physical therapy program often begins with stretching and postural change programs for decreasing the pain. When your pain decreases, more intense exercises directed toward flexibility, power, augmentation of endurance, and a normal life style can be initiated. Exercises must be started as early as possible, as the treatment progresses the exercise schedule must be adapted to it. Learning and keeping up with an exercise and stretching program that can be applied at home is a significant part of the treatment.
Drug Therapy
Drugs used to control pain are called painkillers (analgesics). In most conditions, lower back and leg pain respond to common over-the-counter drugs such as aspirin or acetaminophen. Analgesic-anti-inflammatory drugs, named nonsteroidal antiinflammatory drugs (NSAIDS), may be added in conditions where pain is not controlled with the aforementioned drugs and to control the irritation and inflammation (which is the actual cause of pain) due to disc hernia. These include: ibuprophen, naproxen, diclophenac, and various drugs sold with a prescription. If you have severe and persistent pain, your doctor may give you a short course of narcotic analgesics. In some cases, muscle relaxants are added to the treatment. A higher dose will not give you a faster recovery. Side effects include: nausea, constipation, dizziness, and vertigo—and may lead to addiction. All drugs should be consumed howordered by your doctor. Inform your doctor on all the drugs that you are using. If you previously tried the drugs prescribed to you (including the over-the-counter medicine), tell your doctor whether they worked for you or not.
If your doctor gives you painkillers or anti-inflammatory drugs, watch for side effects such as an upset stomach or stomach bleeding. For problems associated with long-term use of over-the-counter (nonprescribed) or prescribed painkillers and NSAIDs, you’ll need to follow up with your doctor.
There are other drugs with anti-inflammatory effects. Corticosteroids (cortisone) drugs (tablet or injection) are sometimes prescribed for intense lower back and leg pain because of their anti-inflammatory properties. Corticosteroids may have side effects like NSAIDs. You should talk with your physicians about the benefits and risks of these drugs.
Epidural injections or "blocks", may be used to relieve intense leg pain. These are corticosteroid injections made into the epidural space (space around the spinal nerves), and by a doctor trained on this technique. The first injection may be later supplemented with one or two more injections. These are most commonly performed as a part of a comprehensive rehabilitation and treatment program.
Trigger point (where pain is elicited upon pressing) injections of local anesthetic solutions (occasionally corticosteroids may be added) directly onto the painful tissues and muscles along the spine or at the back of the hip bone. Although they are useful for pain control in some conditions, they do not provide correction of the herniated disc.
Surgical Treatment in Lumbar Disc Herniation
The goal of surgery is to prevent the herniated disc from injuring the nerves by pressing on them, therefore from causing symptoms such as pain and loss of power. The most common procedure is discectomy or partial discectomy, removing a piece of the herniated disc. Sometimes a piece of the bone at the back of the disc, named lamina, may have to be removed as well. This is called a hemi-laminotomy if bone removal is minimal, or hemi-laminectomy if bone removal is larger. If the nerve root is irritated after removal of the herniated disc tissue, a complete recovery of pain will be provided.
Recently, surgeons prefer to perform this procedure by using a microscope or endoscope, enabling a small incision that will heal rapidly.
Discectomy may be performed under local, spinal or general anesthesia. The patient is placed prone (facing the bed), and often a position is given that resembles squatting. A small cut is made on the skin located over the herniated disc, and then the muscles on the spine are pulled to the sides. The surgeon may need to remove a small amount of bone to see the compressed nerve. The herniated disc and other torn pieces are removed, without leaving any residual compression on the nerve. The bone projections (osteophytes) are also removed to ensure that the nerve will not be compressed. Bleeding is often minimal.
What Can I expect Post-Surgery?
If your primary complaint is leg pain rather than lower back pain, then you may anticipate a good result from surgery. Before the operation, your doctor will perform an examination and various tests to verify a disc hernia pressing on your nerve is causing the pain. During physical examination, a positive straight-leg-raise test, indicating sciatica, is performed. Muscle weakness, loss of sensation, and changes in reflexes may also be observed. In addition, imaging methods such as MRI (magnetic resonance imaging), CT (computerized tomography), and myelography can clearly show nerve compression. If these tests are positive, your doctor can verify nerve compression and, in that case, a 90 percent probability exists of having an obvious decrease in leg pain after surgery. You should not expect to have a complete absence of pain, however you can live quite a normal life by keeping the pain under control.
Most patients do not experience any complications after discectomy, however similar to every operation, this method carries some risks. Bleeding, infection, injury to the sheath protecting the spinal cord or nerves (dura mater), and injury to the nerves are examples. Also re-rupture of the disc after surgery and relapse of symptoms is possible. In approximately 5 percent of patients, the disc may rupture again and cause symptoms in the future.
Obtain information from your doctor about activity limitations that may be necessary after surgery. Walking around once anesthesia wears off is a good practice. Most patients are discharged within 24 hours following surgery or even the same day. You should avoid driving, sitting for a long time, lifting heavy objects and bending forward for at least four weeks after surgery. Some patients benefit from a therapy program that can be applied under a doctor's counseling. Ask your doctor for back strengthening exercises to avoid facing the same situation again.
When Would I Need Immediate Surgery?
Very rarely, a large disc hernia may impinge on the nerves controlling the bladder and the bowel, resulting in loss of bladder and bowel control. This is generally in association with numbness and tingling in the groin or genital area—requiring urgent disc hernia surgery. Call your doctor immediately if you face such a condition.