Cervical Spinal Stenosis and Treatment
Cervical Spinal Stenosis and Treatment
Cervical Spinal Stenosis and Treatment
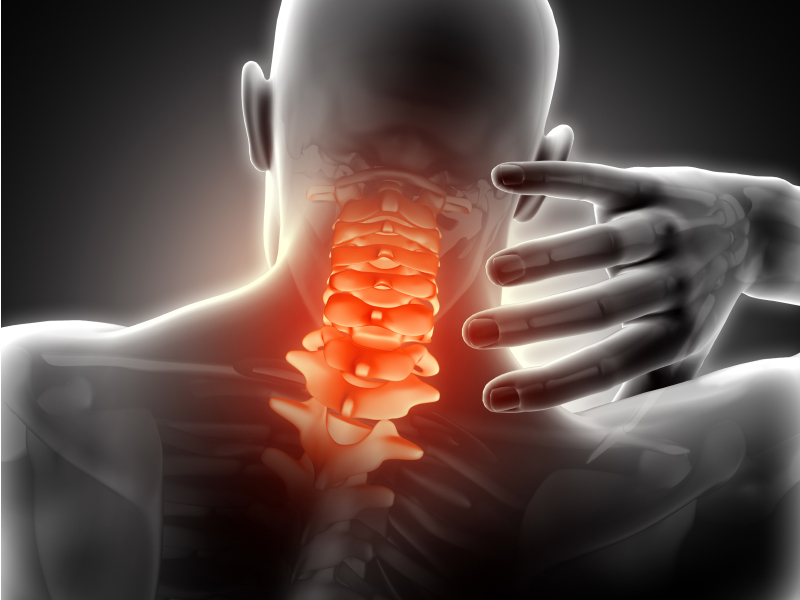
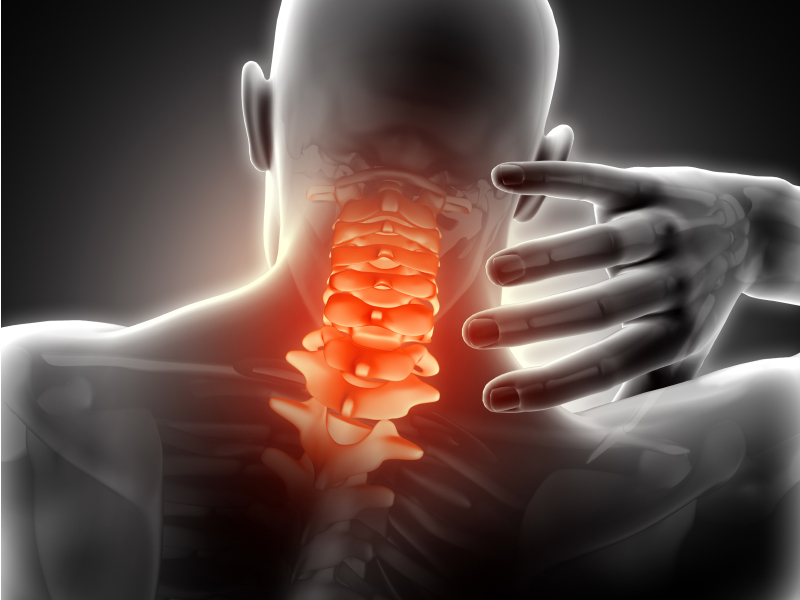
Within the cervical vertebra, a canal exists through which the spinal cord passes. As a part of the normal aging process, discs lose their water content and begin to bulge. In some patients, however, the bulging of the disc and other arthritic changes between the vertebrae constrict the space through which the spinal cord and nerve roots pass. This narrowing results in compression of the spinal cord and nerve roots— called cervical narrow canal or “stenosis”.
Cervical myelopathy: The compression of the cord results in functional loss in the upper and lower limbs. Cervical myelopathy has a progressive course. Handwriting detoriation, dropping objects, and failure to button are frequent complaints. Loss of balance may also occur. In extreme cases, severe weakness and numbness in the arms and legs may exist. More rarely, there may be changes in bowel or bladder control.
Cervical radiculopathy: The compression of the nerve roots resulting in functional loss in a certain part of the extremity. Cervical radiculopathy is pain radiating pain from the neck to the arms, forearms or hands. Muscular weakness may associate in the corresponding muscle groups.
What ıs the Natural Course of Cervical Myelopathy and Cervical Radiculopathy?
The duration of symptoms suggests the natural course. In most the acute cases, symptoms of pain, numbness, and weakness generally disappear within 6-12 weeks. In sub-acute and chronic patients, however, the outcomes vary. In approximately one third of patients, physical therapy and nonoperative care can cause the pain to disappear or reach a level that is tolerable.
For some patients, the pain may be intolerable, thus, requiring further treatment. Although the “natural course” is more uncertain in clinically evident cervical myelopathies, there is a general aggreement that the myelopathy symptoms will progress over time. The rate, timing and rapidity of such a progression, however, are not predictable. Approximately 75 percent of patients show a staged deterioration. In between these “stages,” there may be limited time periods that the symptoms improve. Twenty percent of the patients have a constant worsening, and 5 percenthave rapid worsening.
How Are Cervical Myelopathy and Radiculopathy Diagnosed?
If a stubborn or worsening numbness or weakness is present in your arms and/or legs, you should refer to a spine surgeon. Medical history followed by a physical examination to check the functions of the nerves in your arms or legs, and to check your balance and assess your gait will be performed.
Then radiographic evaluation may follow. X-rays may reveal degenerative changes in the disc spaces or the facet joints. There might also be a slight slippage between the cervical vertebrae. Magnetic resonance imaging (MRI) enables visualization of the soft tissues on the spinal cord or nerve roots that have a possibility of compression. Computed tomography (CT) myelogram that uses contrast material may also be used to enhance viewing the spinal cord.
Electromyogram (EMG) and nerve conduction studies may be used to evaluate the functions of the cord and nerves. These studies help differentiate cervical radiculopathy (illness due to nerve roots) from other nerve diseases in the arm and forearm such as carpal tunnel. Somatic sensory evoked potentials (SSEP) are electrical tests that evaluate signal transduction in the spinal cord, and can be performed in some patients with cervical myelopathy. Follow this link to read about the treatment of cervical spinal stenosis.
Treatment of Cervical Spinal Stenosis
Cervical spinal stenosis is accompanied by myelopathy and/or radiculopathy. Most patients with cervical radiculopathy are initially treated with nonsurgical methods.
The first step in the treatment is “activity modifications”. They are generally simple measures such as adjusting the height of your computer or your chair. Pain medication and local ice or heat applications may also be recommended. Bed rest may be beneficial for a limited period of time. Long-term bed rest is often not recommended since it may negatively affect physical condition and fitness.
Prescribing anti-inflammatory drugs, muscle relaxants, or narcotic painkillers may be the next step when aforementioned precautions are ineffective in pain control. Physical therapy and rehabilitation program is an important part of the healing process and generally will start with also a light stretching and flexibility program as well as informing you about proper ergonomics at home and/or at work. As your pain decreases, mild strenthening exercises may be added to the program.
Epidural steroid injections that are cortisone injections made around the inflamed nerve may be recommended in some patients with cervical root disease. The purpose of the injection is to decrease the inflammation and relieve the pain.
In mild stenosis where the spinal cord is unaffected, nonsurgical treatment may be beneficial. The patients should be careful about avoiding conditions or injuries that may risk their spinal cords. Occupational physiotherapists can make suggestions on daily activities such as bathing, dressing, opening jars, or using keys. If the cervical myelopathy symptoms are evident or progressive, you need to be evaluated by a spine surgeon.
What Are Surgical Options?
When nonsurgical methods are ineffective in relieving pain, surgery is an appropriate alternative. An operation pefomred from the front (anterior), back (posterior), or both may be recommended based on your symptoms. To make the decision on the treatment method, your surgeon will examine you to determine the compression sites in the spinal cord or the nerve roots, and the number of compressed levels. Radiographic and laboratory examinations will help in diagnosing the alignment of your cervical spine and general medical condition. Depending on the type of operation, you may need to wear a collar for a short period.
In the front approach, a small incision is made on the front side of your neck parallel to your skin wrinkles. The tissues will be pulled aside meticulously, and the cervical vertebra will be reached. The disc and tissues compressing the nerve root are removed. A cage is put in between the bones to replace the disc space and the two vertebrae are stabilized to each other with plates and screws. The anterior (front) surgery may be performed at more than one level; it may also require removal of discs and vertebrae.
In the back approach, the incision corresponds to where the nerve roots exit the spinal cord. Bone prominences compressing the nerve will be removed. Small disc fragments can be removed from this hole either via laminectomy or laminoplasty. In laminectomy, the part at the back of the vertebra is completely removed. In laminoplasty, the lamina is elevated on a hinge to reach the space for the spinal cord, which is put back into place at the end of the operation. Sometimes metal screws and plates may be used for stabilizing the spinal column in the neck.